VMAT2 Inhibitors for Tardive Dyskinesia
In this custom video series, key opinion leaders compare VMAT2 inhibitors available for use to treat patients with tardive dyskinesia.
Episodes in this series

Leslie L. Citrome, MD, MPH: Dr Xavier, we do have 2 VMAT2 inhibitors available. What are their names?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: Valbenazine and deutetrabenazine.
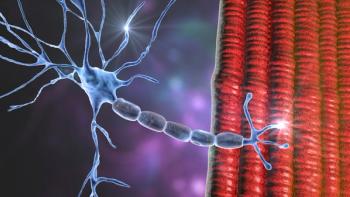
Leslie L. Citrome, MD, MPH: They are very similar, aren’t they? They both produce metabolites that are VMAT2 inhibitors per se, that inhibit the transport of dopamine in neurons. What does that actually do?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: It reduces the dopamine storage because the vesicular monoamine transporters are needed to transport the dopamine from the presynaptic vesicles to the postsynaptic for dopamine action. If there isn’t enough dopamine storage or if valbenazine blocks that, then there’s less dopamine available.
Leslie L. Citrome, MD, MPH: Dopamine, as it sits around in a cell, doesn’t do much. It has to be packaged in those vesicles. If the VMAT2 protein isn’t available to transport that dopamine into the vesicle when the neuron fires, then there isn’t going to be a lot of dopamine being released. That will reduce the dyskinesias that the patient would experience. That’s the thought in terms of the mechanism of action. We have 2 very similar medicines available. There are different terms of what I call the amenities of care. How often do you give it once a day vs twice a day? Do you have to give with food? How are they metabolized? What are the drug-drug interactions? They differ.
Deutetrabenazine, for example, is twice a day with food, and you dose it according to the patient’s needs. It’s very finely dosed. You have a broad range of how you can use this, and you dose it to the point where you have optimal efficacy and tolerability, which is fairly easy to do. With valbenazine, the number of choices of dosing are more limited. It’s once a day, though, with or without food. So that’s a little easier, but it’s metabolized by not only CYP2D6—both are—but also CYP3A4. That means you need to consider another pathway that could be inhibited or induced and that will alter your decision a little in which medicine you might want to prescribe, or basically how you want to dose it. These are more subtle differences.
The bottom line is that both agents work pretty robustly, and the clinical trials are very encouraging. They tell us that the dyskinesias improved quickly and with effects that are noticeable by 6 weeks. The effects are durable with longer exposures. You have ongoing improvement in the dyskinesias that everybody notices. An important aspect of using VMAT2 inhibitors, though—I want to caution our listeners—is that this is a management tool and not a cure. You stop that VMAT2 inhibitor, but it’s likely that the dyskinesias come back. That’s unfortunate that we don’t have a cure, but at least we have a management tool. In the old days, we tried everything. We switched the antipsychotic. We tried to stop the antipsychotic. We gave other medicines that really didn’t work. Now we have VMAT2 inhibitors. That’s a tremendous advance. Any comments about the VMAT2 inhibitors that perhaps I missed?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: No, you’ve covered it all.
Transcript edited for clarity.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.