Case Scenario 1: Patient With Bipolar 1 Disorder Reports New Onset Movements
In this custom video series, experts share overall impressions of a female patient with bipolar 1 disorder who develops new onset movements suggesting tardive dyskinesia and the rationale for intervening with VMAT2 therapy.
Episodes in this series

Leslie L. Citrome, MD, MPH: Welcome to this Psychiatric Times Case-Based Psych Perspectives, expert perspectives on recognition and management of tardive dyskinesia. I am Dr. Leslie Citrome, clinical professor of Psychiatry and Behavioral Sciences at New York Medical College in Valhalla, New York. And joining me is Dr. Rose Mary Xavier, research scientist and psychiatric nurse practitioner with the University of North Carolina at Chapel Hill. Welcome.
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: Thank you. I am happy to be here.
Leslie L. Citrome, MD, MPH: I am happy to have this conversation here. It is very clinically relevant to our audience. The goal of our discussion today is to provide an overview of tardive dyskinesia, as well as offer insights into the management of this detrimental disease. Let’s start by reviewing a couple of case scenarios and try to figure this out. The first one is a patient with bipolar 1 disorder who reports new onset of movements. This is a 54-year-old woman who received a diagnosis of bipolar 1 disorder at the age of 32, after requiring hospitalization for an acute manic episode. She was started on lithium at that time. She relapsed at age 41 with a florid manic episode requiring psychiatric hospitalization, resulting in an atypical antipsychotic being added to her regimen. She presents for routine follow-up. Her only concern relates to feedback received from her husband. About 6 months ago, her husband began observing constant movement of both her hands while watching television in the living room. He had not seen these types of movements by her before, and they seemed to be increasing in degree. He also frequently asked her if she was chewing gum or if she had something in her eye. This case tells us something about a woman exposed to a dopamine receptor blocking agent, that is an antipsychotic, who develops abnormal movements after some delay. It did not happen right away, but over time they became noticeable. Dr. Xavier, what is your overall impression?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: My impression of this case is focusing on the use of antipsychotic medications for treatment of mood disorders, or disorders other than a primary psychotic disorder. When, just reading through this case, there are several things that stand out. Now she is a 54-year-old female. When we look at the risk factors for development of tardive dyskinesia, there are several things that stand out from the studies that have been published. We know that female sex and that the duration of treatment with antipsychotic medications increase the risk for developing tardive dyskinesia. So here we have a 54-year-old female. She has been diagnosed with bipolar disorder. Even though she was started on treatment with lithium, she relapsed at the age of 41 when an atypical antipsychotic medication was added. That is a 13-year history of treatment with antipsychotic medications. And just thinking about, going back to the training period in recent times, we also think about old generation medications, so the first-generation medications would cause tardive dyskinesia. We do not often hear about atypical antipsychotics, but we have data coming in that show that just because a patient is on an atypical medication, it does not diminish the risk for TD [tardive dyskinesia]. The next thing that comes to us is the type of movements that this patient has had. When you look at the case history, we know it has been about 6 months. She has constant movement of both the hands which is increasing in degree progressively, and she has chewing gum type of moments, as well as there is something in her eyes. So talk about the blepharospasm that could occur with TD. She has 4 different types of moments that have been progressively increasing. So it’s a very interesting case, and I look forward to hearing what your thoughts are.
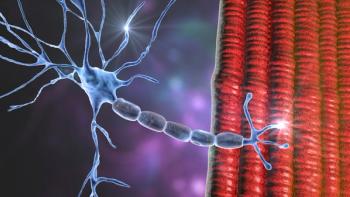
Leslie L. Citrome, MD, MPH: Well, you have highlighted the important points here. She has had a multi-year exposure to an atypical antipsychotic. Atypical antipsychotics today still block postsynaptic dopamine receptors, and we know that is a key ingredient in perhaps the causation of tardive dyskinesia. And her movements, which appeared over time, are delayed. So tardive dyskinesia, tardive delayed dyskinesia, abnormal movement. It all makes sense that that is what we are going to be thinking about in terms of a drug induced movement disorder with her. And I think you pointed out a very important aspect about our treatments today. Although we use atypical antipsychotics, most of the time, they still incur a risk for tardive dyskinesia. They are better in terms of other drug induced movement disorders dramatically, and we do not see as much drug induced Parkinsonism. For example, that rhythmic tremor that appears right after you start an antipsychotic with the shuffling gait or the rigidity, we see a lot less of that. But there is still this liability for tardive dyskinesia. Epidemiological studies tell us that perhaps the prevalence is a little lower with atypical antipsychotics, but it is certainly not zero. My concern with her though is that she is deriving significant benefit from her regimen currently. It is keeping her stable, euthymic. It is preventing the recurrence of mania, which is really devastating for her. It required hospitalization for example. And we know it is very disruptive to functioning. She needs her medicine. And one of the things we cannot really do is stop the antipsychotic. This is what has kept her stable. We need to look at interventions that will allow us to continue her ongoing treatment for her underlying psychiatric disorder. The option in my mind would be something like a VMAT2 [vesicular monoamine transporter type 2] inhibitor, of which two are approved by the FDA [Food and Drug Administration] for the treatment of tardive dyskinesia, which are added to a person's ongoing regimen. If the patient feels secure with their current long-standing regimen, and I'm comfortable with continuing it, and there is a real concern about relapse, that would be my option. And this ties in with our next case where we are going to talk about a patient with tardive dyskinesia who is prescribed a VMAT2 inhibitor.
Transcript edited for clarity.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.