Assessing Severity of Tardive Dyskinesia
In this custom video series, Leslie L. Citrome, MD, MPH, and Rose Mary Xavier, PhD, MS, RN, PMHNP-BC, reference the Abnormal Involuntary Movement Scale (AIMS) rating scale, used to assess the severity of involuntary movements and help diagnose tardive dyskinesia.
Episodes in this series

Leslie L. Citrome, MD, MPH: My question to you Dr. Xavier, how would you monitor someone before and after initiating a VMAT2 inhibitor? What is commonly done in your experience?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: Well once it is prescribed, you also want to know because if someone has parkinsonian-type symptoms or other type of acute or dystonic movement presentations, if you put them on a VMAT2 inhibitor, it can get worse. You also want to monitor the response to the treatment. The other thing is if someone, again before starting any treatment, I think we talked about the importance of assessment. And assessment should include the distribution of movements. For example, where are the movements located? What is the severity of the movements? Once you have done that, it becomes easy to monitor. But for someone who has had a TD [tardive dyskinesia] structured assessment, I know we talked about this earlier, but AIMS [Abnormal Involuntary Movement Scale] is essential. An ongoing assessment is really important. Specifically for VMAT2, I think the most essential thing is to make sure that the movement is not getting worse. And that can offer a differential diagnostic perspective as to: what exactly were you treating? Or did you, and some of these movements are, have so much common characteristics? Some can be complex in presentation. Because we can have patients who have tardive dyskinesia who also have parkinsonian-type tremor. The systemic and the neurological presentations that are common that are seen with patients who have schizophrenia who are at an advanced age, it can be very hard to tease that apart.
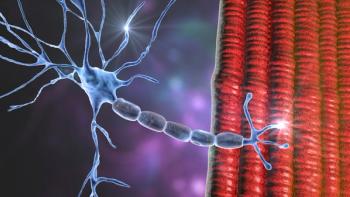
Leslie L. Citrome, MD, MPH: A structured assessment would be very helpful in figuring out what that person has. And we did talk a little bit before we started recording about what structured assessments are out there. And you had mentioned to me that you had worked in Minnesota. And in Minnesota they have developed this instrument called the DISCUS. I forget exactly what that acronym stands for, but it is not really used elsewhere. And you had mentioned that you use the Abnormal Involuntary Movement Scale, the AIMS, and that is pretty much the gold standard. It is used in the clinic. It is also used as an outcome measure in research in the development of medicines for tardive dyskinesia. The AIMS, the Abnormal Involuntary Movement Scale, examination should be familiar to most of our listeners. And if not, you should learn about it. It is a standard structured way to assess for tardive dyskinesia and other movements. And it has specific instructions. It does not take very long to do maybe 5 to 10 minutes. But it does require methodically going over several body parts looking for movements and eliciting them through something called activation maneuvers where we ask patients, for example, to touch their thumb to their fingers as quickly as they can while observing their face, to open their mouth and stick out their tongue to look at the facial dyskinesias. We look at their hands, we look at their feet, and we look at their trunk. We look to see how they walk. And all these abnormal movements that we detect the dyskinesias, we can rate on a scale of 0 to 4. Let me mention that scale for a moment for our listeners. Zero means no movement when you rate a muscle group. One is there is a movement or maybe there is not, I’m really not sure. A two is a movement that we can all agree that we see, but it is not dramatic. A three, is a movement that everyone will notice, you cannot miss it. And a four, you cannot miss it from across the parking lot. So, 0 to 4. And there are 7 muscle groups that are systematically reviewed during an AIMS exam. And there is nothing complicated about it. Four of these muscle groups are actually the face. So different parts of the face including the tongue and the jaw. And then there is one item that rates all the upper extremities. Both arms and both hands. There is an item for both legs and feet. And there is a separate item for the trunk. And that is it. And if you just can see dyskinesias in any of these 7 muscle groups, you rate them from 0 to 4. And that gives you an idea of where the dyskinesias are and how severe they are. The overall severity of the dyskinesia is rated on item 8 of the AIMS. Remember that item 8 global assessment. And it is the highest rating you gave for any of the muscle groups you just looked at. And that gives you a sense of the dyskinesia severity. The other items of the AIMS will tell you the, ask you to rate the patient's distress level and awareness, as well as impairment on function. And there are items also that remind us to ask about their dental status and whether they have dentures. And it sounds complex, but it really is very simple and in one sheet of paper. The instructions though for the AIMS help us figure out, is this tardive dyskinesia, or is this drug-induced Parkinsonism, or is this both? And how can I say that you are wondering, because none of the items that we rate actually rate drug-induced Parkinsonism. Here is where the instruction for the AIMS is important to keep in mind. The instructions tell us to do a whole bunch of other things. It does not take long to do, but it tells us look on how the patient walks. If they have a shuffling gait or reduced arm swing, that means they have some degree of rigidity and perhaps drug-induced Parkinsonism. We do not rate that on the form, we just look for it. And the AIMS instructions tell us to do that. The other thing the AIMS instructions tell us to do is extend and flex the patient’s upper extremities to check for stiffness. And if you see cogwheeling like this, then that makes you think of drug-induced Parkinsonism.
Transcript edited for clarity.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.