Not All That Writhes Is Tardive Dyskinesia
Some dyskinesias improve with antipsychotic treatment, and these types are more common than thought. More in this podcast.
Dr Aiken is Instructor in Clinical Psychiatry at the Wake Forest University School of Medicine and the Director of the
RESEARCH UPDATE
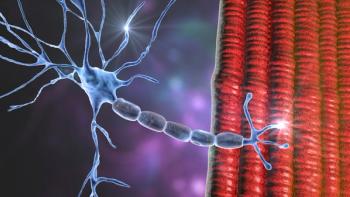
There are two types of tardive dyskinesia (TD), and understanding the difference is essential in this era where this once hopeless syndrome is now treatable. The reason is that one of them may not respond to medications in the way we expect. This “type” is actually not TD at all-it is spontaneous dyskinesia (SD).
SDs were first described in patients with schizophrenia by Emil Kraeplin and Eugen Bleuler in the early 1900s. They are part of the disease process of schizophrenia and occur in patients who have never taken antipsychotics, as well as those who have. They look identical to TD, but are not caused by antipsychotics, whereas TD by definition is a consequence of antipsychotic exposure.1 In fact, SDs tend to improve with antipsychotics because they are part of the disease process itself.2
How do we know they are part of the disease process? SDs wax and wane, as does TD, but the spontaneous ones rise with the intensity of the psychotic symptoms and fall when they improve. When psychosis is worse, they get worse. These dyskinesias are part of the genetic vulnerability to schizophrenia. Though rare in the general population, SDs are seen in schizotypal personality disorder and are two to three times more common in the first-degree relatives of patients with schizophrenia.1,3
SDs are fairly common in schizophrenia and worsen with the duration of illness. Prevalence rates in patients with schizophrenia are low (4%) at the start of the illness but rise to 40% in antipsychotic-naïve patients over age 60.1 They are rare in the general population, occurring at a rate of 29 per 100,000 life years, but more common in the elderly and those with brain injuries.4 TD is also more prevalent in those groups, leading some to speculate that TD and SDs share a common etiology.1 However, this doesn’t explain the elevated risk of TD in affective disorders, where SDs are virtually absent.
What it means for treatment
The new VMAT2 inhibitors for TD-valbenazine and deutetrabenazine-were developed to address part of the known pathophysiology of TD: dopaminergic hypersensitivity. They are effective for TD, with a number needed to treat (NNT) between 4 and 7.5 But will they work for SDs? After all, these dyskinesias have a different etiology and may arise from different biological pathways. SDs improve, rather than worsen, with antipsychotics. How they will respond to VMAT2 inhibitors is an open question, but a neglected theory of schizophrenia may point the way toward an answer.
That theory is dopamine hypersensitivity. There is evidence from biological and family studies that hypersensitivity of the dopamine system is a risk factor for schizophrenia, and that it plays a causative role in SD just as it does in TD.1 If that is true, the SDs would improve with VMAT2 inhibitors, and psychosis may improve with these agents as well.6 Indeed, one of the first medications for psychosis, and one that actually preceded the antipsychotics, was reserpine; a VMAT2 inhibitor.7
The bottom line
TD is ripe with paradox. SDs actually improve with antipsychotics, while TDs may appear to improve, because antipsychotics can mask tardive movements through their Parkinsonian effects.8 As part of the disease process, SDs may worsen when antipsychotics are discontinued. TD can worsen during antipsychotic withdrawal as well, in the form of withdrawal dyskinesias.7 With all of this uncertainty, measurement is essential.
Before starting a VMAT2 inhibitor, rate the symptoms with an
References:
1. Tenback DE, van Harten PN. Epidemiology and risk factors for (tardive) dyskinesia. Int Rev Neurobiol. 2011;98:211-230.
2. Peralta V, Campos MS, De Jalón EG, et al. Motor behavior abnormalities in drug-naïve patients with schizophrenia spectrum disorders. Mov Disord. 2010;25:1068-1076.
3. Mittal VA, Neumann C, Saczawa M, et al. Longitudinal progression of movement abnormalities in relation to psychotic symptoms in adolescents at high risk of schizophrenia. Arch Gen Psychiatry. 2008;65:165-171.
4. Merrill RM, Lyon JL, Matiaco PM. Tardive and spontaneous dyskinesia incidence in the general population. BMC Psychiatry. 2013;13:152.
5. Solmi M, Pigato G, Kane JM, et al. Treatment of TD with VMAT-2 inhibitors: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2018;12:1215-1238.
6. Skaff R. Valbenazine and Deutetrabenazine as possible treatments for neuroleptic-induced supersensitivity psychosis and antipsychotic dependence. CNS Spectr. 2018:1-2.
7. Goldberg JF and Ernst CL.
8. D'Abreu A, Akbar U, Friedman JH. TD: Epidemiology. J Neurol Sci. 2018;389:17-20.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.