
The authors summarize findings from the first study to compare suicide risk for veterans who do and those who do not use VA services.

The authors summarize findings from the first study to compare suicide risk for veterans who do and those who do not use VA services.

If forgiveness soon after trauma helps avert mental disorders or retaliation, how could the aftermath of the Charleston tragedy not end up being one of the great moments of forgiveness in history?

The patient did not just scream for more medication-he literally rolled on the floor, ranting and raving and demanding higher doses. Some may write him off as an "addict," but this case reaffirms the value of studying medicine before practicing psychiatry or psychopharmacology.

The author applies psychodynamic psychology to understand and recognize so-called "homegrown" terrorists, individuals who are familiar with American culture and thus more difficult to detect.

Neither facile liberal censure nor rabid applause from the right speak to Eastwood’s purposes in this superbly crafted picture.
In most movies, psychiatrists are depicted in a negative light, which most certainly affects our public image. Was the psychiatrist in American Sniper portrayed positively or negatively?

Today, we embrace the collective experiences of our fellow members of the human race, this Holocaust Remembrance Day and 70th Anniversary of Auschwitz liberation.

The privacy and security of our offices-the therapeutic bunkers within which our wounded patient-warriors hunker down against an unseen enemy-is the fundamental first barricade between private sufferings and the potential for public humiliation.
People experience a spectrum of reactions as a result of epidemics, such as Ebola, and disasters, such as weather-related events. Psychiatrists can provide interventions for those who are in distress with a special focus on mitigating these disaster stress reactions.

This sunflower at the 9/11 Memorial said that a ray of sunshine remains, and that life blooms anew, in spite of the losses.

Military veterans are ubiquitous in our practices and in our lives. The impact of the past several years of armed conflict is greater than many think-and much greater than simply the number of veterans in your practice or your community.

Maltreatment at an early age casts a very long shadow. Here: a look at the long-term effects of early childhood trauma.

Substantial progress has been made in the development of etiologic models of intimate partner violence and interventions for individuals who assault their intimate partners. These authors provide details.

This book is the first scholarly work that attempts to fill the enormous gap in the conventional armamentarium used to treat PTSD.

The limited effectiveness of current approaches provide compelling arguments for effective conventional and complementary interventions aimed at preventing PTSD and treating chronic PTSD. Specifics here.

We do not have to set time aside to do something that helps validate our experience, while simultaneously coping with it. The lesson expressed in this psychiatry resident's poem.
Those who have experienced extreme trauma and their descendents have taught us much about resilience, renewal, and redemption-outcomes that are all recalled in this period of the Jewish Passover, Christian Easter, and Holocaust Memorial Week.

When Wordsworth rhapsodized about yellow flowers, it is doubtful that he expected his verse to translate into the mental health realm. Yet that is exactly what happened.

In the history of psychiatry, the First World War is often identified with the rise of the disorder of “shellshock.” However, many in both the medical community and the military establishment were dubious of the claim that war could produce psychiatric symptoms.

It is clear from a 21st century psychiatric perspective that Augustine was suffering from PTSD, but Augustine was victimized in ways far more horrific than filmmaker Alice Wincour revealed. More in this film review by Alan Stone, MD.
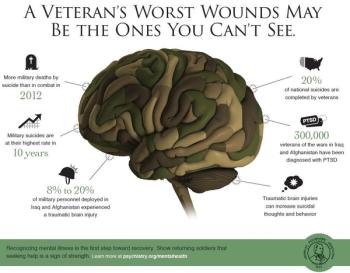
The invisible wounds of war continue to infiltrate the minds and consciousness of veterans and their families, as shown in this infographic and public service announcement by the APA, featuring by Rep. Patrick Kennedy.

This child's behaviors suggested ADHD-combined or primarily hyperactive type and conduct disorder. However, there was a strong history of trauma and affective disturbance. A structured interview format indicated that he formally met criteria for both PTSD and mixed episode. Without this format, features defining these disorders might have been missed and the child treated only for ADHD.

Here, suggestions for mental health professionals serving the needs of refugees from around the world who have been traumatized by violence.

This article highlights several features of medical and social importance that are somewhat unique to the Somali refugee community in the US.

If our survey on medical cannabis is any indication, psychiatrists are widely-and deeply-divided on whether and how marijuana should be used in clinical practice. You can read the results here.